
Heart palpitations
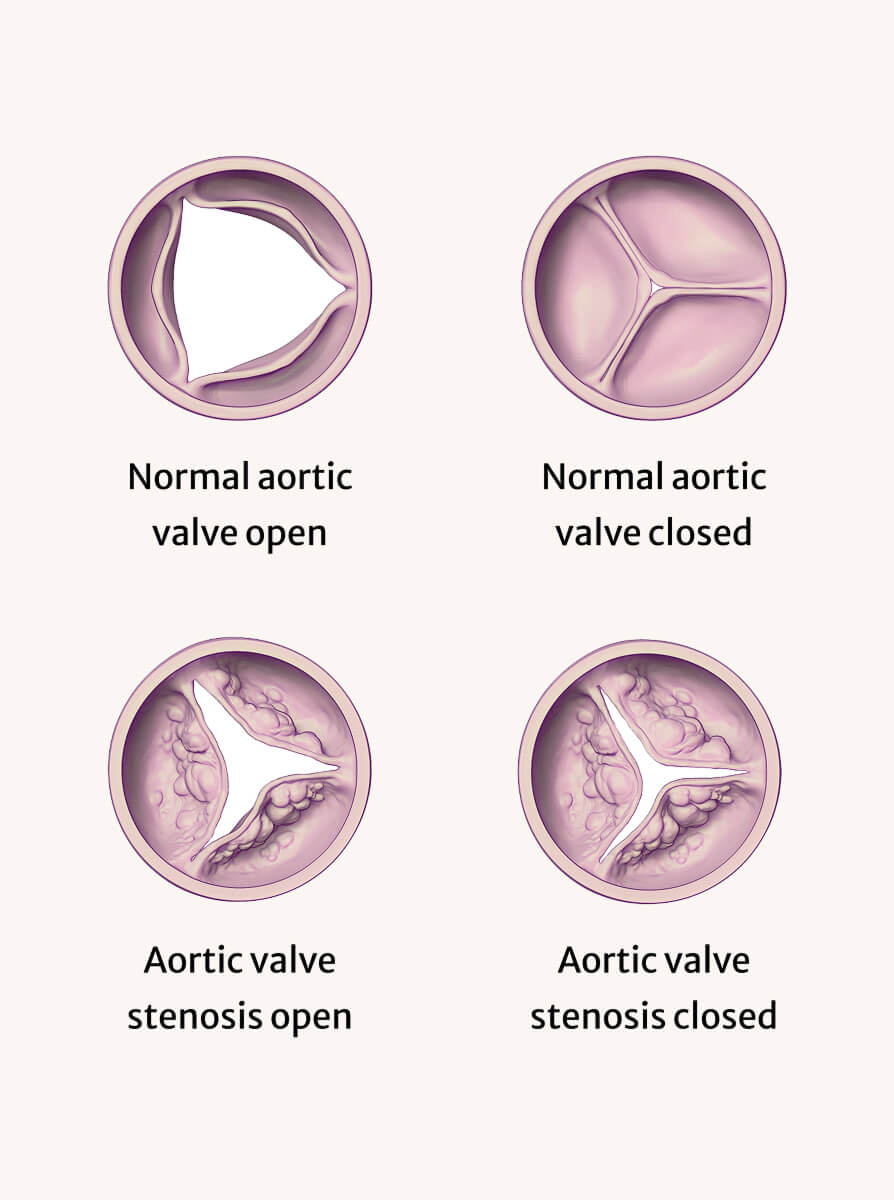
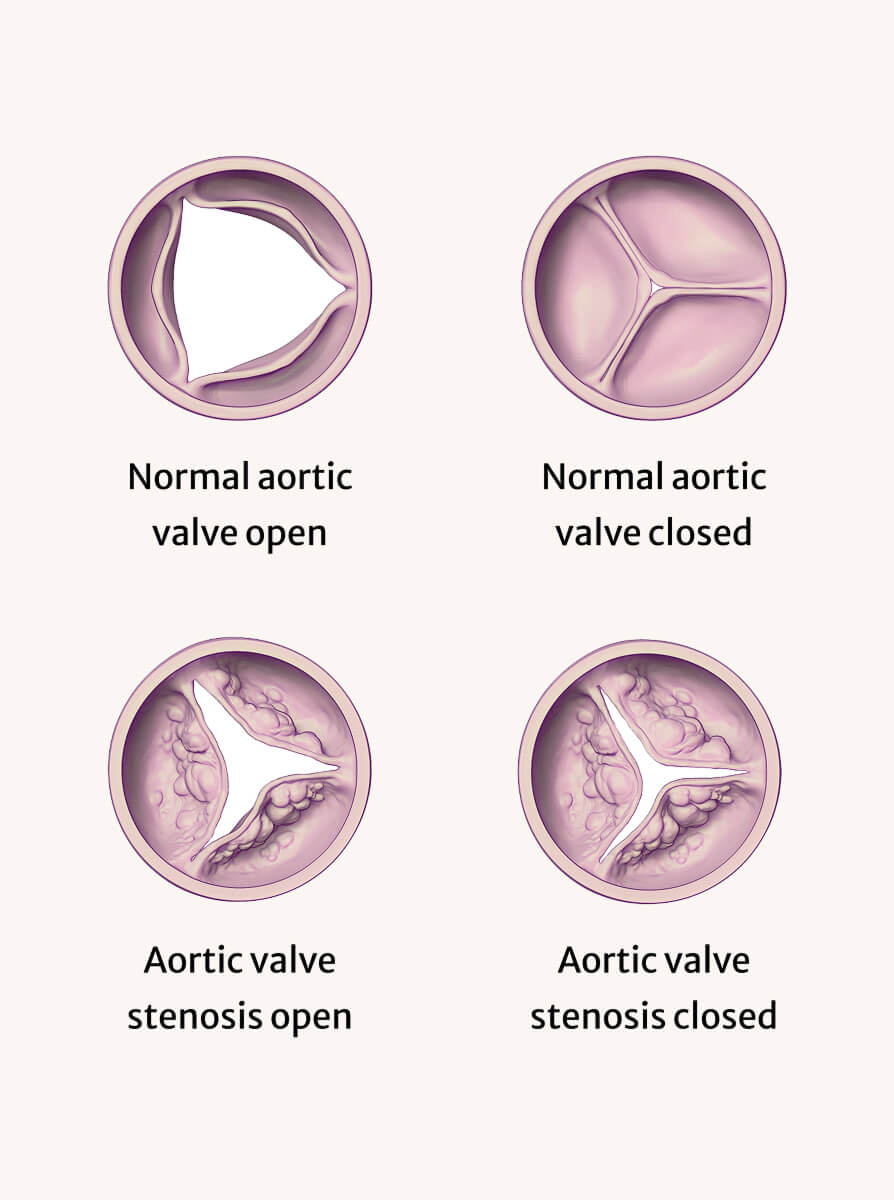
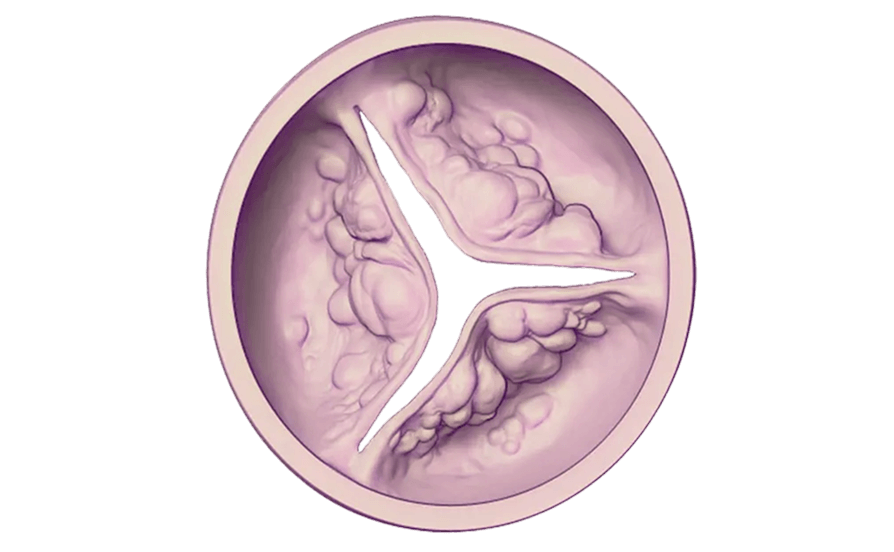
Aortic Stenosis is a condition in which the aortic valve, which controls blood
flow from the heart to the rest of the body, becomes narrowed or blocked.
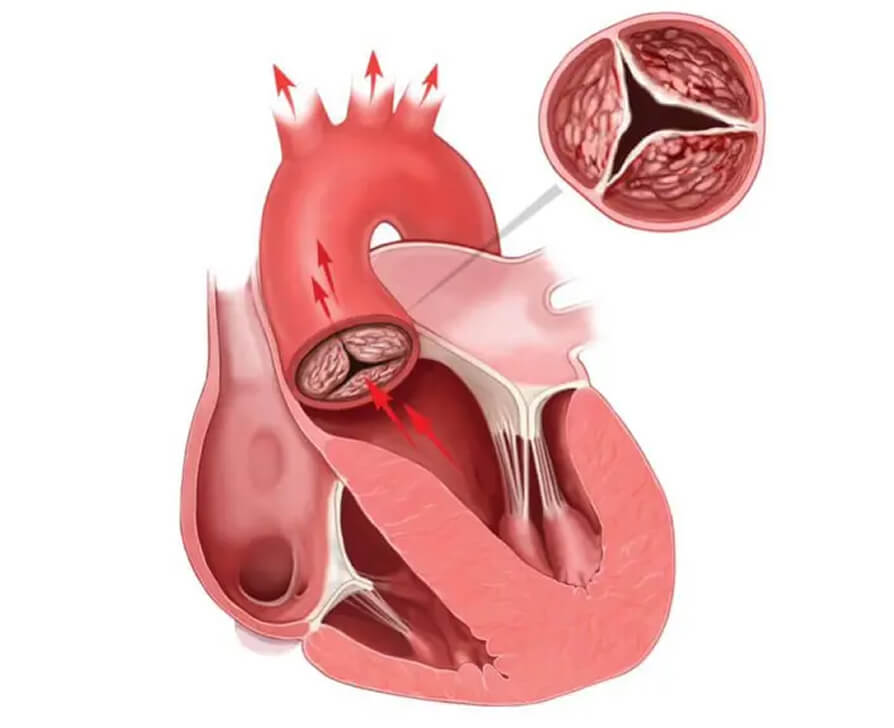
In case of Aortic Stenosis, the aortic valve becomes narrower or stiffer, which can make it harder for blood to flow through the valve and into the aorta.
As the aortic valve becomes narrower, the heart has to work harder to pump blood through the valve and into the aorta. This can cause the left ventricle of the heart to become thicker and less flexible, which can eventually lead to heart failure if left untreated.1
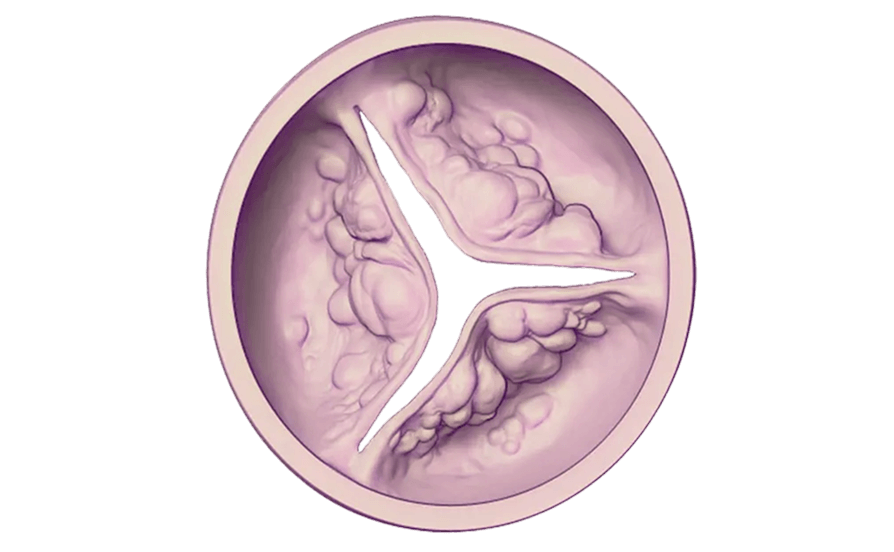
Age related calcium build up on the aortic valve: Calcium can leave our bones and move into the wrong places as we get older, and the most common cause of Aortic Stenosis is calcium building up on the valve making it stiff and restricting the amount of blood that can flow through.3
You may have Aortic Stenosis and not experience symptoms for many years. As it becomes more severe, your symptoms may include:

Heart palpitations

Shortness of breath

Sudden weight gain

Trouble doing usual activities/exercise

Dizziness of fainting

Chest pain

Ankle swelling

Extreme tiredness

Fever or night sweats
In the mild and moderate stages of Aortic Stenosis, the decrease in blood flow is usually not significant enough to cause obvious symptoms. In fact, many people are unaware they have the condition as symptoms can often be mistaken as normal signs of aging. When Aortic Stenosis becomes severe, it means that the narrowing of the aortic valve has become significant enough to impede blood flow out of the heart. This can lead to several serious symptoms or complications, including:
It's important to note that in some cases, severe Aortic Stenosis may not cause noticeable symptoms, especially in older adults who may have reduced activity levels. However, even in the absence of symptoms, severe Aortic Stenosis can still pose a significant risk of complications. This is why regular monitoring, Echocardiograms (Echos) and prompt treatment are crucial for managing Aortic Stenosis.3,4
Your GP will usually do the initial examination. If a heart murmur is heard or they suspect you may have a problem with one of your valves your GP will refer you for an Echocardiogram (Echo) or directly to a cardiologist.
Aortic Stenosis can be diagnosed using several methods. These may include:
Fictional Characters
Aortic Stenosis is a progressive disease, which means it usually gets worse over time. Because of this, doctors will typically measure it as mild, moderate, or severe. The stage of aortic stenosis depends on how damaged your valve is.
Your healthcare team will monitor your valve and how your heart is pumping. This is done through regular medical visits, Echocardiograms (Echos) and other tests.
During early stages of the disease (mild or moderate), your doctor may decide to watch your condition. If it worsens, you will need to have your valve replaced. When your Aortic Stenosis requires intervention, your doctor will review all of the options available to you. If not, ask.
Aortic Stenosis is often progressive so follow up Echos are important to see if your disease has progressed.
Every 3 to 5 years
Every 1 to 2 years
Every 6 to 12 months3
You and your doctor may:
If your Aortic Stenosis is severe and you have symptoms for example, chest pain, fainting, shortness of breath, and fatigue, or your heart function has worsened aortic valve replacement may be your recommended treatment option.
You may also need to take certain medications to treat other heart disease risk factors and/or prevent clots or infections of the heart valve.
It can be hard to remember everything you want to tell your doctor. Use our symptom tracker to make notes, to share with your doctor.

Fictional Character

Fictional Character
You can manage early symptoms with medication and a healthy lifestyle. When the symptoms become severe or your heart function declines, your doctor may recommend replacing the damaged valve.1
We’ve got answers. Our FAQ page can help guide you through, symptoms, what to expect from a check up and what treatments are available.

Note: References provided are applicable for all medical claims on this page.
Information on this site includes educational information regarding certain conditions and potential therapies or treatment options. Other therapies or treatment options may be available and you should discuss any educational information you access online with your healthcare professional. Appropriate treatment for individuals is a matter for healthcare professionals to decide in consultation with each individual.